References
The following organizations were referenced for this article. Specific references are provided below each recommendation. Further information about each organization is available here.
- World Health Organization (WHO)
- US Department of Health and Human Services (HHS)
- US Department of Health and Human Services Eunice Kennedy Shriver Institute of Child Health and Human Development (NICHD)
- Centers for Disease Control and Prevention (CDC)
- American College of Nurse-Midwives (ACNM)
- American College of Obstetricians and Gynecologists (ACOG)
- March of Dimes
- Star Legacy Foundation
- Tommy’s
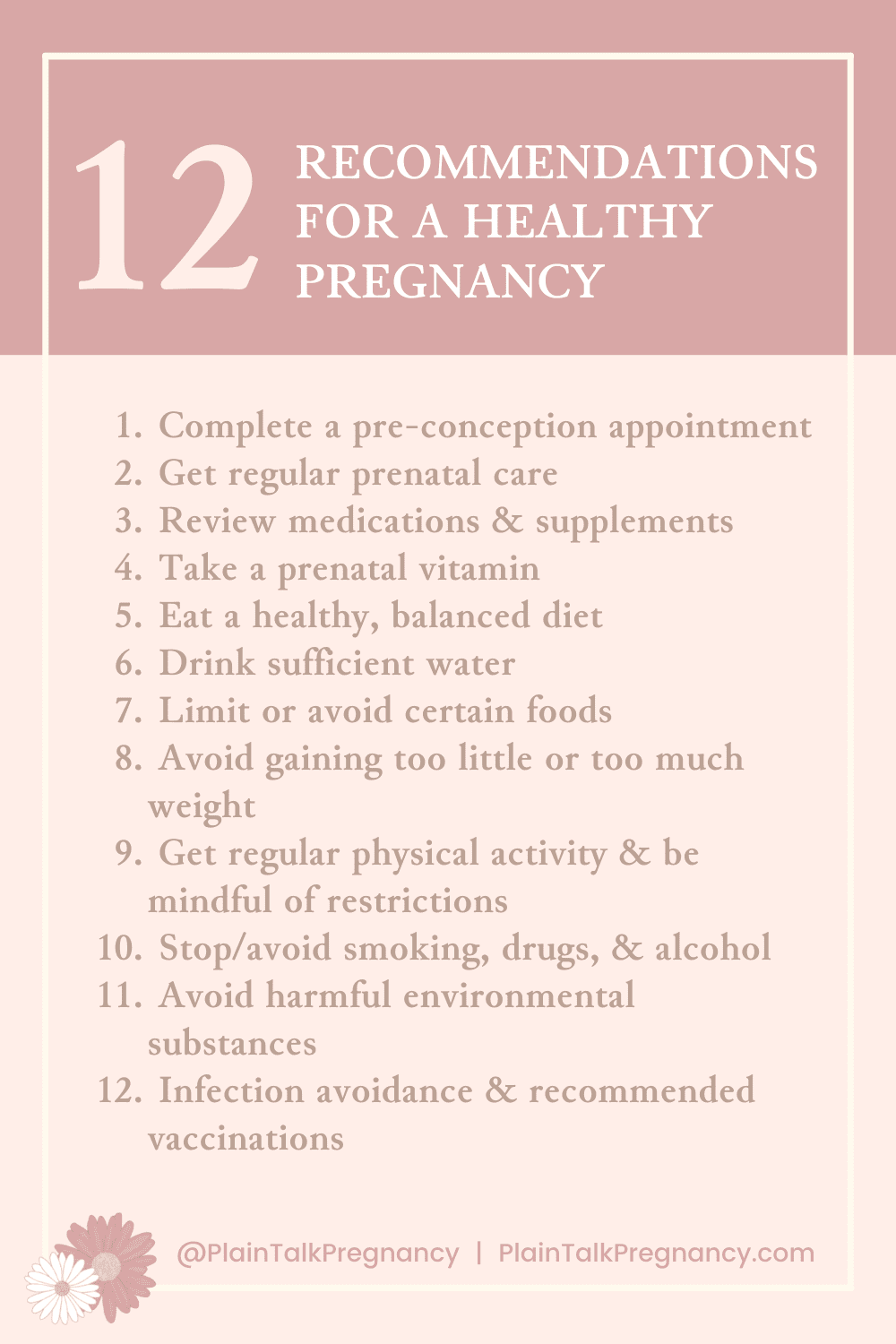
Recommendations for a Healthy Pregnancy
This section is a survey of high-level information about current recommendations for a healthy pregnancy. Many of the individual recommendations listed here will be explored more in-depth in follow-on articles.
As part one of a two-part series, this piece is focused on recommendations that are generally agreed upon in the prenatal care community. Part two of the series will explore more specialized recommendations that may not be covered or may not be agreed upon by all major sources within the community.
Please note that recommendations specific to the COVID environment have not been included in this article. Plain Talk Pregnancy recommends you discuss any COVID-related concerns with your individual prenatal provider.
1. If possible, complete a pre-conception appointment with your provider
Visit your primary care provider or your obstetric/women’s health provider. Use this visit to discuss family and medical history, current medications and supplements, management of preexisting conditions, and any other aspects of your life or medical care that could affect a pregnancy. It is recommended to conduct a preconception visit even if you have had a child previously.
You can also decide about genetic screening at this time.
Specific References
WHO: N/A for this recommendation. (Did we miss it? Let us know)
HHS: Preconception health
NICHD: What is prenatal care and why is it important? | Can you promote a healthy pregnancy before getting pregnant?
CDC: Planning for Pregnancy | Family Health History and Planning for Pregnancy
ACNM: The Role of the Certified Nurse-Midwife/Certified Midwife in Preconception Health and Health Care (Position Statement) (Note: Includes general thoughts on preconception healthcare, but is not specifically a recommendation for a preconception visit or preconception planning)
ACOG: Your Pregnancy and Childbirth (book) Chapters 1 and 23 | Good Health Before Pregnancy: Prepregnancy Care
March of Dimes: Planning Your Pregnancy (General information on planning for pregnancy) | Getting Ready for Pregnancy: Preconception Health | Your Checkup Before Pregnancy
Star Legacy Foundation: Safer Pregnancy | Stillbirth Prevention: Parenting in Pregnancy (Brochure)
Tommy’s: N/A for this recommendation. (Did we miss it? Let us know)
Plain Talk Note: A preconception visit can be a good idea, but if your pregnancy was not planned, many of these items can be discussed during an initial prenatal visit as well.
2. Get regular prenatal care
Schedule and attend regular visits with your chosen prenatal care provider. Attend visits even if you feel well, as complications can be identified during routine checks. You can also use the time with your provider to discuss your questions and concerns.
Visits may include height and weight measurements, blood pressure and urine checks, measurement of your fundal height (your belly) and your baby’s heartbeat, general physical wellness exams, and potentially a pelvic exam. Based on your individual medical circumstances, some visits may also include recommended testing and procedures.
Specific References
WHO: Who Recommendations (book) Recommendation E (Note: specifically discusses midwifery continuity of care model, but is acknowledged as a context-specific recommendation. Also see Plain Talk Pregnancy’s notes on WHO in our reference page) | Recommendations on Maternal Health #1 (same note as previous) | Promoting Healthy Pregnancy | Quality antenatal care infographic (minimal information)
HHS: Prenatal care and tests
NICHD: What is prenatal care and why is it important? | What are some common complications of pregnancy? | Other Pregnancy FAQs | About Pre-Pregnancy Care and Prenatal Care | What happens during prenatal visits?
CDC: Commit to Healthy Choices to Help Prevent Birth Defects
ACNM: Evidence-Based Prenatal Care Visits: When Less is More (Note: Discusses evidence for a lower-frequency schedule of prenatal visits specifically for low-risk gestating parents)
ACOG: Your Pregnancy and Childbirth (book) Chapters 2 and 4 (Note: ACOG discusses timing of prenatal visits, but does not emphasize importance of prenatal care. Plain Talk Pregnancy believes this to be an oversight in phrasing, but we want to acknowledge what is written.)
March of Dimes: Prenatal Care | Prenatal Care Checkups | Birth Defects and Your Baby
Star Legacy Foundation: N/A for this recommendation. (Did we miss it? Let us know)
Tommy’s: 5 things to do when you find out you’re pregnant (Discusses importance of contacting provider right away after determining you are pregnant) | Your antenatal appointment schedule | Antenatal care
3. Review Prescription & OTC Medications and Supplements
In conjunction with your provider, review all current prescriptions medications and make changes if required. Review medications even if you have taken them previously with no complications. Do not start or stop a new prescription without discussing with your provider. There may be circumstances where the benefits of continuing a medication outweigh the risks of using it during pregnancy, but this decision is best made in conjunction with your provider. Your provider may recommend you start, stop, or continue prescription medications based on your specific medical circumstances. You may also need to adjust your dosage based on increased weight during pregnancy.
Also discuss over the counter (OTC) medications and skincare items with your provider. Some OTCs are not recommended for use during pregnancy, and some interfere with prescription medications you may be taking. Retinoids (a type of skin care product) are not recommended during pregnancy. Your provider should be able to provide a list or specific recommendations of over-the-counter medications that are safer to use.
Finally, although many supplements are available over the counter, some supplements may have an affect on your pregnancy. Review your supplements with your provider as well.
Specific References
WHO: N/A for this recommendation. (Did we miss it? Let us know)
HHS: Preconception health | Staying healthy and safe
NICHD: What is prenatal care and why is it important? | Other Pregnancy FAQs | What can I do to promote a healthy pregnancy?
CDC: Planning for Pregnancy | Treating for Two: Medicine and Pregnancy; Providing Better Information to Women and Healthcare Providers | Commit to Healthy Choices to Help Prevent Birth Defects
ACNM: Taking Medicine During Pregnancy
ACOG: Your Pregnancy and Childbirth (book) Chapters 1, 3, 4, 24, and 27 | Reducing Risks of Birth Defects | What medicine can I take for allergies while I’m pregnant? | Skin Conditions During Pregnancy
March of Dimes: Prenatal Care Checkups | Getting Ready for Pregnancy: Preconception Health | Your Checkup Before Pregnancy | Prescription Medicine During Pregnancy | Prescription Opioids During Pregnancy | Preventing NAS in Your Baby (Infographic) | Over-the-Counter Medicine, Supplements and Herbal Products During Pregnancy | Isotretinoin and Other Retinoids During Pregnancy | Birth Defects and Your Baby
Star Legacy Foundation: Stillbirth Prevention: Parenting in Pregnancy (Brochure)
Tommy’s: 5 things to do when you find out you’re pregnant | Drugs and medicines in pregnancy
4. Take a prenatal vitamin
In conjunction with your provider, choose a prenatal vitamin that best fits your needs. Ensure your vitamin includes 400-600mg of folate or folic acid to aid in reduction of neural tube defects (NTD). Prenatal vitamins should also include vitamins A, C, and D, and may include iron.
Some vitamins included in prenatals are dangerous at higher doses. For this reason, do not take more than the recommended dose of your prenatal vitamin. If you need additional amounts of a specific vitamin, add a supplement in addition to your prenatal vitamin.
Pay attention to the instructions, as some brands or types of vitamins should be taken multiple times or at certain times during the day.
Some people may have trouble stomaching prenatal vitamins, especially in early pregnancy. If this is the case, work with your provider to try different brands or try taking your vitamin at different times in the day. There are also gummy vitamins or other alternatives available that may be easier on your stomach.
Specific References
WHO: Who Recommendations (book) Recommendation A (Note: WHO recommends supplementation of some nutrients, but also recommends sourcing other nutrients through a balanced diet) | Recommendations on Maternal Health #1 (Same note as previous)
HHS: Preconception health (Specifically about folic acid) | Staying healthy and safe
NICHD: What is prenatal care and why is it important? (Specifically about folic acid) | Can you promote a healthy pregnancy before getting pregnant? (Specifically about folic acid) | What are some common complications of pregnancy? (Discusses iron-deficiency anemia) | What can I do to promote a healthy pregnancy? (Specifically about folic acid and iron) | What health problems can develop during pregnancy? (Specifically about iron)
CDC: Folic Acid | Folic Acid Helps Prevent Some Birth Defects | Commit to Healthy Choices to Help Prevent Birth Defects
ACNM: Taking Good Care of Yourself While You Are Pregnant | Folic Acid
ACOG: Your Pregnancy and Childbirth (book) Chapters 1, 3, 22, and 24 | Nutrition During Pregnancy | Reducing Risks of Birth Defects
March of Dimes: Vitamins and Other Nutrients During Pregnancy | Folic Acid | Folic Acid Health Action Fact Sheet | Prenatal Care Checkups | Birth Defects and Your Baby | Getting Ready for Pregnancy: Preconception Health | Eating Healthy During Pregnancy | Anemia
Star Legacy Foundation: Stillbirth Prevention: Parenting in Pregnancy (Brochure) (Recommendation to discuss folic acid and other vitamins and supplements with provider)
Tommy’s: What supplements do I need in pregnancy? (Specifically, folic acid and Vitamin D) | Benefits of taking folic acid before pregnancy | 5 things to do when you find out you’re pregnant (General recommendation to take vitamins) | Dos and don’ts for a safer pregnancy (Specifically, folic acid and Vitamin D)
5. Eat a healthy, balanced diet
Eat a healthy, balanced diet incorporating all five food groups. Ensure you consume sufficient amounts of protein, folate, calcium, iron, and fiber, and limit excess sugar and fats.
If you have a special diet or dietary needs, discuss it with your prenatal provider. They may also refer you to a dietician.
Although you need to increase your caloric intake to provide nutrients for your growing child, avoid “eating for two”; for most expecting parents, caloric intake should not increase by more than a few hundred calories/day.
Specific References
WHO: Who Recommendations (book) Recommendation A | Recommendations on Maternal Health #1
HHS: Staying healthy and safe
NICHD: What is prenatal care and why is it important? | What are some common complications of pregnancy? (Discusses iron-deficiency anemia) | Can you promote a healthy pregnancy before getting pregnant? | What can I do to promote a healthy pregnancy?
CDC: N/A for this recommendation. (Did we miss it? Let us know)
ACNM: Taking Good Care of Yourself While You Are Pregnant | Folic Acid | Preventing Iron Deficiency Anemia During Pregnancy
ACOG: Your Pregnancy and Childbirth (book) Chapters 1, 4, 6, 22 | Nutrition During Pregnancy
March of Dimes: Nutrition, Weight, and Fitness | Getting Ready for Pregnancy: Preconception Health | Vitamins and Other Nutrients During Pregnancy | Folic Acid | Folic Acid Health Action Fact Sheet | Anemia
Star Legacy Foundation: Safer Pregnancy | Stillbirth Prevention: Parenting in Pregnancy (Brochure) (Recommendation to discuss nutrition with provider)
Tommy’s: Benefits of taking folic acid before pregnancy | 5 things to do when you find out you’re pregnant (General recommendation to eat healthy) | How to eat well in pregnancy | How much should I eat during pregnancy? | 7 tips for eating well in pregnancy | Healthy eating tips | Questions about weight in pregnancy
6. Drink sufficient water
Water not only aids in normal bodily processes during pregnancy, but it also helps to form the amniotic fluid around the baby. You should aim to drink between 64-96 ounces of water per day during pregnancy. Ensure to drink water before and during exercise or physical exertion.
Specific References
WHO: N/A for this recommendation. (Did we miss it? Let us know)
HHS: Staying healthy and safe
NICHD: What can I do to promote a healthy pregnancy?
CDC: N/A for this recommendation. (Did we miss it? Let us know)
ACNM: Taking Good Care of Yourself While You Are Pregnant
ACOG: Your Pregnancy and Childbirth (book) Chapters 22 | How much water should I drink during pregnancy? | Nutrition During Pregnancy
March of Dimes: Eating Healthy During Pregnancy
Star Legacy Foundation: N/A for this recommendation. (Did we miss it? Let us know)
Tommy’s: How much water should I drink in pregnancy? | 7 tips for eating well in pregnancy | Healthy eating tips
7. Limit or avoid certain foods
Certain foods are not recommended during pregnancy, and certain others are recommended in limited quantities.
Limit caffeine to 200mg or less daily. This is approximately the amount found in a large cup of coffee. Remember that caffeine is also present in soda, some teas, and even chocolate.
Avoid seafoods that are high in mercury, which has been linked to birth defects. Also avoid raw or seared fish.
Limit sodium and salt intake to 2300mg or less each day. Check labels because sodium can be found in surprising places.
Use simple sugars and sugar substitutes in moderation.
Because gestating parents are more susceptible to foodborne illnesses, additional foods to be avoided include those which can carry listeria bacteria, salmonella bacteria, campylobacter bacteria, and escherichia coli (E. coli) bacteria. These foods include:
- Unpasteurized or raw milk or juice
- Soft cheeses
- Hot dogs or deli meats
- Raw or undercooked seafood, meat, or poultry
- Raw or undercooked eggs
- Foods or surfaces contaminated with raw poultry
- Raw sprouts or unwashed fruits and vegetables
- Infected water
It is also important to practice food safety, thoroughly clean dishes and surfaces, and disinfect surfaces between uses to avoid cross-contamination.
In additional to not drinking alcohol during pregnancy (see #10) below, gestating parents should also avoid foods cooked in alcohol.
Specific References
WHO: Who Recommendations (book) Recommendation A (Note: specifically discusses caffeine; also, WHO recommends limiting caffeine to 300mg or less, as opposed to the 200mg figure used elsewhere) | Recommendations on Maternal Health #1 (also specifically about caffeine)
HHS: Staying healthy and safe
NICHD: What can I do to promote a healthy pregnancy?
CDC: People at Risk – Pregnant Women and Newborns (Listeria)
ACNM: Taking Good Care of Yourself While You Are Pregnant | Eating Safely During Pregnancy
ACOG: Your Pregnancy and Childbirth (book) Chapters 22 and 25 | Nutrition During Pregnancy | Listeria and Pregnancy | How much coffee can I drink while pregnant?
March of Dimes: Nutrition, Weight, and Fitness | Eating Healthy During Pregnancy | Foods to Avoid or Limit During Pregnancy | Caffeine in Pregnancy | Mercury and Pregnancy | Birth Defects and Your Baby
Star Legacy Foundation: N/A for this recommendation. (Did we miss it? Let us know)
Tommy’s: 5 things to do when you find out you’re pregnant (General recommendation to avoid certain foods and limit caffeine in pregnancy) | Foods to avoid in pregnancy | Food poisoning and pregnancy | Limiting your caffeine intake in pregnancy | Dos and don’ts for a safer pregnancy
8. Avoid gaining too little or too much weight
Weight gain during pregnancy should be gradual, starting slowly in the first trimester, and increasing steadily in the second and third trimester. There are risks both to gaining too much and too little weight during pregnancy. Work with your provider to monitor and adjust your weight gain as needed.
Specific References
WHO: Who Recommendations (book) Recommendation A | Recommendations on Maternal Health #1
HHS: Staying healthy and safe
NICHD: What is prenatal care and why is it important? (General recommendation to follow a healthy diet) | Other Pregnancy FAQs | What can I do to promote a healthy pregnancy?
CDC: Weight Gain During Pregnancy
ACNM: Weight Gain During Pregnancy
ACOG: Your Pregnancy and Childbirth (book) Chapters 1 and 22 | Nutrition During Pregnancy
March of Dimes: Nutrition, Weight, and Fitness | Weight Gain During Pregnancy | Eating Healthy During Pregnancy
Star Legacy Foundation: N/A for this recommendation. (Did we miss it? Let us know)
Tommy’s: Weight management in pregnancy | How much weight should I gain in pregnancy?
9. Get regular physical activity & be mindful of physical restrictions
Getting regular physical activity during pregnancy can help to reduce discomforts of pregnancy, and can also help to reduce complications.
Regular physical activity
Consult with your provider on the activities that are safest to perform during your pregnancy, and incorporate approximately 30 minutes of regular physical activity into most days. If 30 minutes at a time is not feasible, break it up into smaller chunks of time.
Always make sure to warm up and drink plenty of water.
Use caution and reduce or stop exercises that cause discomfort or pain. If an exercise triggers vaginal bleeding, uterine contractions, fluid from vagina, swelling in calf muscles, blurred vision, faintness, shortness of breath, chest pain, headache, stopped or decreased fetal movement, or any other pregnancy-related concerns, it is best to stop the activity and call your provider immediately.
Sports and exercises to avoid
Because of physical changes brought on by pregnancy, certain activities that involve bouncing or jarring motions or the potential for physical injury are not recommend. These include sports with a risk of impact or falling, activities in a heated environment such as hot yoga, activities at high altitude, and SCUBA diving, among others.
You may also want to avoid certain types of movements in normal activities, such as lying flat on your back in later pregnancy. In addition, based on your individual medical considerations, some gestational parents will be advised on additional restrictions.
Daily activities to minimize or avoid
Certain daily activities may be recommended against as well, particularly in later pregnancy. These include heavy lifting, climbing, carrying, and standing for long periods, among others. If you perform these activities at work, work with your employer and your prenatal provider on reasonable accomodations for your circumstances.
Traveling while pregnant is generally okay, but gestating parents should be aware of the possibility of deep vein thrombosis (DVT). DVT is a blood clot, generally in the legs, that may be dislodged and travel to the lungs. In order to prevent DVT, drink sufficient water, get out of your seat regularly, and stretch and move while you travel. You may also discuss the use of compression socks with your provider. If traveling by car, always wear your seatbelt.
It is also recommended to avoid raising a gestating parent’s core body temperature pregnancy. For this reason, it recommended to avoid or minimize exposure to hot tubs and saunas, and to work with your provider to determine an appropriate temperature for bath water.
Specific References
WHO: Who Recommendations (book) Recommendation A, D (Note: discusses importance of exercise, but does not discuss activities to be avoided) | Recommendations on Maternal Health #1 (Same note as previous)
HHS: Staying healthy and safe
NICHD: What is prenatal care and why is it important? (General recommendation for getting exercise during pregnancy) | What can I do to promote a healthy pregnancy? (Recommends discussing physical activity during pregnancy with provider)
CDC: Commit to Healthy Choices to Help Prevent Birth Defects | Healthy Pregnant or Postpartum Women | Pregnant Travelers
ACNM: Taking Good Care of Yourself While You Are Pregnant | Exercise in Pregnancy
ACOG: Your Pregnancy and Childbirth (book) Chapters 1, 3, 9, 23, 24, and 26 | Exercise During Pregnancy | Travel During Pregnancy | Car Safety for Pregnant Women, Babies, and Children | Preventing Deep Vein Thrombosis
March of Dimes: Getting Ready for Pregnancy: Preconception Health | Nutrition, Weight, and Fitness | Exercise During Pregnancy | Travel During Pregnancy | Seatbelts During Pregnancy
Star Legacy Foundation: Safer Pregnancy | Stillbirth Prevention: Parenting in Pregnancy (Brochure) (Recommendation to adopt an active lifestyle)
Tommy’s: All about exercise in pregnancy | Making a plan for exercising in pregnancy | 10 tips for staying active in pregnancy | Exercises to avoid in pregnancy | Pregnancy and Work (Specifically about physical limitations during pregnancy; Note: Also discusses some workers rights issues that are specific to the UK) | 5 things to do when you find out you’re pregnant (General recommendation to stay active) | Dos and don’ts for a safer pregnancy | Staying healthy at work during pregnancy | Can I fly in pregnancy?
10. Stop/avoid smoking, drugs, & alcohol
Cigarettes, drugs, and alcohol use can result in complications during pregnancy, including preterm birth, low birth weight, and stillbirth. They may also result in higher incidents of Sudden Infant Death Syndrome (SIDS) after birth. Alcohol consumption during pregnancy can result in Fetal alcohol spectrum disorder (FASD), whose effects can last a lifetime.
Avoid smoking, illegal drugs, and alcohol during pregnancy. If you currently smoke, drink, or use illegal drugs, quit. If you have trouble quitting, there are treatment programs that can help. If you live with or spend time with someone who smokes, work with them to quit as well.
Vaping, or e-cigarettes, are not a safe alternate to smoking tobacco.
Although legal in some jurisdictions, marijuana use during pregnancy may pose risks to the baby as well.
Specific References
WHO: Who Recommendations (book) Recommendation B | Recommendations on Maternal Health #1
HHS: Preconception health | Staying healthy and safe
NICHD: What is prenatal care and why is it important? | Other Pregnancy FAQs (Specifically about not smoking during pregnancy) | Can you promote a healthy pregnancy before getting pregnant? | What can I do to promote a healthy pregnancy? | Substance Use While Pregnant and Breastfeeding
CDC: Planning for Pregnancy | Substance use During Pregnancy | Commit to Healthy Choices to Help Prevent Birth Defects | Smoking, Pregnancy, and Babies | Pregnant? Don’t Smoke! | Secondhand Smoke | What You Need to Know About Marijuana Use and Pregnancy | Alcohol use in Pregnancy | Fetal Alcohol Spectrum Disorders (FASDs)
ACNM: Environment Hazards During Pregnancy | Taking Good Care of Yourself While You Are Pregnant | Smoking and Women’s Health: Tips on Why and How to Quit | Alcohol and Pregnancy | Substance Use Disorders in Pregnancy (Position Statement)
ACOG: Your Pregnancy and Childbirth (book) Chapters 1, 3, 22, 24 | Reducing Risks of Birth Defects | Tobacco, Alcohol, Drugs, and Pregnancy | Alcohol and Women | Alcohol and Pregnancy | It’s Time to Quit Smoking | Tobacco and Pregnancy | Marijuana and Pregnancy | Opioid Use Disorder and Pregnancy
March of Dimes: Prenatal Care Checkups | Getting Ready for Pregnancy: Preconception Health | Your Checkup Before Pregnancy | Birth Defects and Your Baby | Is It Safe? | Alcohol During Pregnancy | Fetal Alcohol Spectrum Disorders | Smoking During Pregnancy | Street Drugs During Pregnancy | Marijuana and Pregnancy | Prescription Medicine During Pregnancy | Prescription Opioids During Pregnancy | Preventing NAS in Your Baby (Infographic) | Air Pollution (Discusses second-hand smoke) | Cocaine and Pregnancy | Heroin and Pregnancy
Star Legacy Foundation: Safer Pregnancy | Stillbirth Prevention: Parenting in Pregnancy (Brochure)
Tommy’s: Dos and don’ts for a safer pregnancy | 5 things to do when you find out you’re pregnant (Specifically discusses smoking and alcohol in pregnancy) | Can I drink alcohol during pregnancy? | Foetal alcohol syndrome | Smoking and pregnancy | Get help to stop smoking | Drugs and medicines in pregnancy | Illegal or recreational drugs and pregnancy | Mums-to-be should talk openly to their midwives, not be shamed into silence (Discusses substance use and addiction)
11. Avoid harmful environmental substances
Exposure to certain environmental substances can be harmful or more harmful during pregnancy and should be avoided. These substances include lead, mercury, pesticides, and radiation.
Environmental Toxins
Lead exposure may affect brain development during pregnancy. Lead is sometimes found in soil, older homes, and in older consumer products, and is currently used in some decorative dishes, jewelry, hobbies, and some manufacturing jobs. Lead may also be found in water coming from older pipes or from wells. Gestating parents should avoid working with or being around sources of lead. If lead exposure is suspected, work with your provider to get a blood test to confirm.
Some gestating parents experience a craving for soil, often caused by anemia or a nutrient deficiency. Lead exposure may occur from eating soil or other non-food items, and should be avoided.
Mercury may affect nervous system development during pregnancy. Mercury is found in certain types of fish, in some thermometers, older consumer items, some light fixtures, and in some workplaces. When eating fish, focus on those with lower levels of mercury. You can check local authorities for recommendations.
Exposure to certain pesticides may affect brain development during pregnancy. It is recommended to avoid using pesticides inside the home during pregnancy, and also to thoroughly wash produce before eating. It is also recommended to avoid chemical flea products for your pets.
Some additional environmental concerns include arsenic, solvents, and second-hand smoke. Ensure the cleaning products you use are safe for use during pregnancy, and ensure adequate ventilation during use.
Radiation
Radiation is present in several aspects of normal life, from dental or other medical x-rays, to airline travel. High doses or cumulative amounts of radiation may affect a developing fetus, but the risks should always be weighed against the benefits.
If you require a medical x-ray during your pregnancy, ensure your providers and technicians are aware you are pregnant. They will follow recommended guidelines regarding protective draping, and may offer alternatives where they exist.
Contrast agents (basically, special dies) are sometimes used during x-rays or during magnetic resonance imaging (MRI). Because it is unknown at this time if contrast agents are harmful during pregnancy, the general recommendation is to avoid them unless medically necessary.
Radiation exposure increases at higher altitudes used in airline travel. For the average person, this is not a big concern; however, if you fly frequently, it may be worth discussing with your provider.
Exposure via the Workplace
The above recommendations are applicable to exposure for gestating parents in the course of their daily lives. However, some gestating parents work with these substances on a regular basis. If this is the case for you, work with your employer on accommodations to minimize your exposure during pregnancy.
Specific References
WHO: N/A for this recommendation. (Did we miss it? Let us know)
HHS: Preconception health | Staying healthy and safe
NICHD: What can I do to promote a healthy pregnancy?
CDC: Radiation Emergencies | Radiation Emergencies and Pregnancy | Reproductive Health and the Workplace; Pregnancy and You Job
ACNM: Environment Hazards During Pregnancy
ACOG: Your Pregnancy and Childbirth (book) Chapters 24, 25, and 26 | Good Health Before Pregnancy: Prepregnancy Care | Travel During Pregnancy
March of Dimes: Getting Ready for Pregnancy: Preconception Health | Your Checkup Before Pregnancy | Birth Defects and Your Baby | Being Pregnant at Work | Lead Poisoning | Mercury and Pregnancy | Solvents and Pregnancy | Radiation and Pregnancy | Air Pollution
Star Legacy Foundation: N/A for this recommendation. (Did we miss it? Let us know)
Tommy’s: Chemicals and pregnancy (Discusses chemicals, but not lead, mercury, or radiation) | Staying healthy at work during pregnancy (Discusses accomodations at work)
12. Infection avoidance and recommended vaccinations
Certain infections can pose a risk during pregnancy, either to the gestating parent and/or to the developing fetus. These include group b streptococcus (GBS), cytomegalovirus (CMV), hepatitis, human immunodeficiency virus (HIV; the virus that causes AIDS), human papillomavirus (HPV), measles, meningitis, mumps, pneumococcal pneumonia, rubella, syphilis, toxoplasmosis, varicella (chickenpox), zika virus, and many sexually transmitted diseases (STD), among others.
Gestating parents are advised to avoid exposure whenever possible. Exposure may be avoided or minimized by following food safety and sanitation guidelines at home, avoiding travel to areas where infections are common, avoiding close contact with infected individuals, and by avoiding illegal drugs and practicing safe sex. Specifically for the avoidance of toxoplasmosis, gestating parents are advised to have another household member empty any cat boxes in the home.
Some infections may also be prevented through the use of a vaccine. While some vaccines are not recommended during pregnancy, others are. Gestating parents should discuss available vaccines with their provider and consider getting the ones recommended for their specific circumstances. If the gestational parent is not currently pregnant, they may consider being vaccinated prior to attempting pregnancy.
Gestating parents should especially consider the Tetanus, Diphtheria, and Pertussis (TDaP) vaccine during each pregnancy, and if pregnant during flu season, the Influenza vaccine as well. Depending on your specific medical circumstances, other vaccines may be recommended by your provider.
Specific References
WHO: Who Recommendations (book) Recommendation B (Note: Discusses HIV, STD testing, and TB), and Recommendation C (GBS, Tetanus, Malaria) | Recommendations on Maternal Health #1 (discusses vaccines and certain infections) and #4 (discusses additional infections) | WHO publishes new estimates on congenital syphilis | Zika Virus Fact Sheet
HHS: Preconception health | Prenatal care and tests | Pregnancy Complications
NICHD: What are some common complications of pregnancy? | What infections can affect pregnancy? | Other Pregnancy FAQs (Discusses seasonal flu and flu shot) | Can you promote a healthy pregnancy before getting pregnant? (General recommendation on being up to date on vaccines) | What can I do to promote a healthy pregnancy? (Infections during pregnancy) | What health problems can develop during pregnancy? (Infections during pregnancy)
CDC: Planning for Pregnancy | Commit to Healthy Choices to Help Prevent Birth Defects | What You Need to Know About Marijuana Use and Pregnancy | Guidelines for Vaccinating Pregnant Women | Pregnancy and Vaccination Fact Sheet | You can start protecting your baby from whooping cough before birth Fact Sheet | Pregnant? You Need a Flu Shot! | 10 Tips for Preventing Infections Before and During Pregnancy | Pregnancy and HIV, Viral Hepatitis, STD, & TB Prevention
ACNM: Infections | Vaccines and Pregnancy | Immunization in Pregnancy and Postpartum (Position Statement) | Preventing Pertussis (Whooping Cough) | Vaccines for Adults | Sexually Transmitted Infections (STIs) (not specific to pregnancy) | Group B Strep in Pregnancy
ACOG: Your Pregnancy and Childbirth (book) Chapters 1, 8, and 25 | Good Health Before Pregnancy: Prepregnancy Care | Reducing Risks of Birth Defects | The Flu Vaccine and Pregnancy | Why should I get Tdap during pregnancy? | Urinary Tract Infections (UTIs) | Group B Strep and Pregnancy | Hepatitis B and Hepatitis C in Pregnancy | Protecting Yourself Against Hepatitis B and Hepatitis C | HIV and Pregnancy | Zika Virus and Pregnancy (video) | Zika Virus and Pregnancy (infographic)
March of Dimes: Prenatal Care Checkups | Getting Ready for Pregnancy: Preconception Health | Your Checkup Before Pregnancy | Vaccinations and Pregnancy | Birth Defects and Your Baby | Caring for Pets When You’re Pregnant (Offers additional information about rodents and reptiles) | Chickenpox During Pregnancy | Cytomegalovirus and Pregnancy | Group B Strep Infection | HIV and Pregnancy | Influenza (Flu) and Pregnancy | Rubella and Pregnancy | Syphilis in Pregnancy | Toxoplasmosis | Zika Virus and Pregnancy (Infographic)
Star Legacy Foundation: N/A for this recommendation. (Did we miss it? Let us know)
Tommy’s: Vaccinations in pregnancy | Infections in pregnancy
Plain Talk Notes:
- Due to the numerous and varied types of infections, we could not go in depth on this recommendation. Future articles will discuss individual infections, as well as options for prevention, avoidance, and treatment.
- Plain Talk Pregnancy adheres to general medical guidelines regarding routine vaccination. We understand individuals many choose differently; however, discussion on efficacy or desirability of routine vaccination is outside the scope of the Plain Talk Pregnancy mission.
- Plain Talk Pregnancy is not discussing the COVID vaccine at this time. We recommend discussing this vaccine with your individual provider.
Human Factors
Plain Talk Pregnancy believes it’s important to consider the human factors relevant to any recommendations in pregnancy. Such factors include elements of time, money, and emotional impact, among others. Consideration of human factors helps to provide context and results in a more fully-informed environment for all expecting parents. Read more in our “About” page.
Human factors relevant to this article include:
Planned vs. unplanned pregnancy
The first recommendation covered in this article concerns preconception planning and counseling. Although a preconception visit can be a great idea, it is not always possible—according to the Guttmacher Institute, as many as 45% of all pregnancies in the United States are not planned (2011 statistics).
What does this mean for you? 1. If your pregnancy was unplanned, you’re not alone; and 2. If you weren’t able to attend a preconception visit, many of the items discussed there can be discussed during your first prenatal appointment. In particular, ensure you go over your medical history, review all medications, and talk to your provider about a prenatal vitamin or any other needed supplements.
Healthcare coverage and access
Another important statistic to be aware of is that between 11-14.2% of US residents don’t have health insurance (Census Bureau, Household Pulse Study, 2020-2021 and ongoing; numbers are likely impacted by the COVID environment but are not widely different than previous years). Additionally, even when insured, insurance doesn’t always meet individual needs, including prescriptions or vitamins.
If you are struggling with healthcare coverage or struggling with access to the coverage you need, there are programs available to help. Please see the resources listed in the “Resources & Additional Reading” section or call 1-800-311-BABY (1-800-311-2229). You can also receive nutrition assistance through programs like WIC.
Time
Another barrier to prenatal care is the issue of time. Gestating parents who work during business hours may feel reluctant to sacrifice work hours for routine appointments, particularly if they don’t have options for paid time off. If this is the case for you, it may be worth discussing with your provider, as some providers will offer late appointments one or two days per week. Additionally, some employers may be open to alternate hours to make up for any time missed for appointments.
Another option is to look into the Family and Medical Leave Act (FMLA). “The FMLA entitles eligible employees of covered employers to take unpaid, job-protected leave for specified family and medical reasons with continuation of group health insurance coverage under the same terms and conditions as if the employee had not taken leave.” Time off for prenatal care falls under FMLA. Although time off under FMLA is not paid, employees may use accrued benefits such as sick leave to receive pay for this time.
History of Trauma
Another factor to be aware of is how a history of trauma can impact a gestating parent’s desire to receive healthcare or consent to specific procedures. Pelvic exams in particular may be triggering during pregnancy. If this is the case, ACOG offers some thoughts on potential ways to make an exam more bearable. You also have the option to refuse pelvic exams should you wish.
Previous pregnancy loss may also complicate a gestating parent’s feelings about prenatal care and pregnancy in general. Plain Talk Pregnancy will be offering a future article on ways to cope during pregnancy after loss. Tommy’s also offers some suggestions, via their articles on Pregnancy after a miscarriage, Pregnant after a stillbirth or late term loss, and Pregnancy after neonatal loss.
Finally, gestating parents who have struggled with eating disorders or disordered eating in their past may find themselves reluctant to agree to weight checks during prenatal visits. If this applies to you, it is recommended that you discuss this with your prenatal provider. Under these circumstances, providers may arrange “blind” weight checks, where they keep track of your weight for medical purposes, but do not inform you of the actual numbers unless necessary. Although it may be tempting to forgo weight checks entirely, please consult with your provider before making this decision.
Resources & Additional Reading
While Plain Talk Pregnancy plans to break down each of these recommendations in further detail in future articles, we have also provided the below links for additional reading and resources:
- Are there any health assistance programs for pregnant women, mothers, and children? (HHS)
- Behavioral Health Treatment Services Locator (HHS)
- Family and Medical Leave Act (US Department of Labor)
- Food Safety for Moms to Be (FDA)
- Know Your Family Health History (American Society of Human Genetics)
- Pregnancy and Breastfeeding (MyPlate, USDA)
- Medicine and Pregnancy (FDA)
- MotherToBaby.org – Information about safety during pregnancy
- Healthy Bodies, Healthy Babies – Information about eating disorders and pregnancy
- Rape, Abuse & Incest National Network (RAINN)
- Rethinking Drinking; Alcohol and Your Health (NIH)
- Smokefree.gov
- Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) (USDA)
What’s up Next?
This article covered the generally accepted recommendations for a healthy pregnancy. Part Two is going to analyze some of the more recent and specialized recommendations, including fetal movement tracking and recommended position for sleeping, among others.
Do you have a specific question or concern you’d like to see examined by Plain Talk Pregnancy? Do you have any additional thoughts on this article or things we might have missed? Contact us or comment below.